Pregnancy Period: Various Types of High Risks In Pregnancy

Pregnancy and its Related Risks
Although the pregnancy won’t be considered high risk just because someone is above 35, the age does mean that you might be more likely to have or to develop a problem that results in extra monitoring, tests or treatment. Some conditions develop during the pregnancy such as high blood pressure, make the pregnancy high risk from the start. Various types of high risk pregnancies are discussed below in detail.
Gestational diabetes is a disorder of sugar (glucose) regulation that occurs specifically in pregnancy. It means that the body’s ability to regulate sugar levels is not up to the strain of pregnancy.
Normally, sugar levels are regulated by a balance between two hormones insulin (produced in the pancreas) and glucagon (made by the liver). Insulin is released when the blood sugar levels rise after eating, allowing the body to remove excess sugar from the bloodstream. Glucagon is released when the blood sugar levels are low, triggering a rise in blood sugar levels.
-
Diabetes And Labor
Women with gestational diabetes requiring treatment are at increased risk of having a large baby, the risk depends partly on how well blood sugars are controlled during the pregnancy. If someone has diabetes, the doctor will usually estimate baby’s birth weight before going into the labor, either by feeling baby through the uterus or using ultrasound. If the baby is normal size, the physician may induce labor at 39 weeks because of the increased risk of fetal complications in prolonged pregnancy in women with diabetes. During labor, it will need to have an IV and blood sugar levels will be carefully monitored every hour or two. If baby’s weight is more than 9-9½1b (4 to 4.5kg) there is a risk that the shoulders may get stuck (known as shoulder dystocia), which increases the chance of a birth injury or other serious complications. The physician will talk to the patient about this risk and may offer a cesarean delivery.
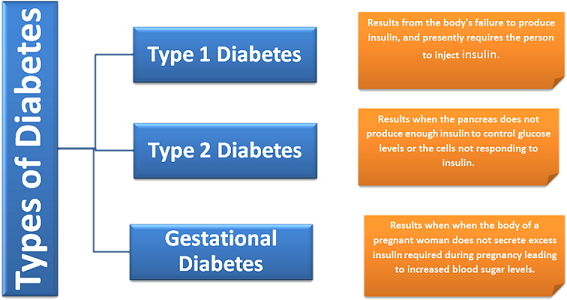
Type Of Diabetes
In gestational diabetes, the body either fails to produce enough insulin to cope with the strain of pregnancy or body’s cells are resistant to insulin’s action. This is similar to type 2 diabetes (sometimes called adult onset diabetes). Type 1 diabetes, which usually begins in childhood or adolescence is different in that the pancreas doesn’t make any insulin. During pregnancy, person’s placenta produces a hormone called human placental lactogen (HPL), which makes blood sugar levels rise. As a result of this, the body has to produce more insulin to maintain normal sugar levels. Gestational diabetes will disappear after pregnancy is over, but the person is much more likely to develop type 2 diabetes later.
How Is It Diagnosed?
Gestational diabetes is initially detected in the third trimester of pregnancy by a one-hour glucose test i.e. a screening test to identify women at a higher risk of sugar problems. Women who are found to be at risk, then her diagnostic test called a glucose tolerance test to determine whether or not they have gestational diabetes. This test is very similar to the one-hour test, but a patient has to get her blood drawn four times instead of just once. Blood glucose levels are checked when the person hasn’t eaten anything (fasting), then 1, 2, and 3 hours after you drink a second sugar drink. If the blood sugar levels are high after 3-hour glucose test, it means the body was not able to handle a sugar load and person have gestational diabetes. Different care providers may use slightly different sets of criteria to diagnose gestational diabetes based on the blood test. Some doctors may consider a particular glucose tolerance test result borderline, while others will want to monitor and treat this actively.
How Is It Treated?
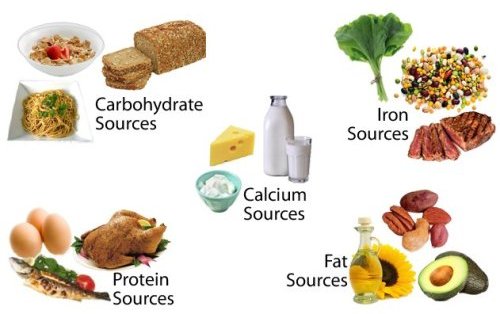
In most cases, gestational diabetes can be treated by adjusting the diet to reduce the carbohydrate in take. Hiring a dietitian can be costly, for more cost effective tips read a resource page here. The care provider may suggest to see a nutritionist, who will advise that what one can and cannot eat. The person is likely to be told to eat unrefined, complex carbohydrates such as wholemeal bread, rice, and pasta and to avoid cakes, sodas, and sweets. The care provider will monitor the blood sugar on her new diet. The blood sugar may have to be tested up to four times a day at home, and it will be expected to do this testing by using a simple, handheld glucose monitor. If the blood sugars remain high, one will need to have insulin injections (twice a day injection) or possibly a glucose-lowering pill.
Some Recommended Food items
Future Risk Of Diabetes
If someone develops gestational diabetes during the pregnancy, she is more likely to develop type 2 diabetes later in life. She should be tested for diabetes with a blood test (after another glucose drink) 6 weeks after the pregnancy, and then at regular intervals after that week. A small ultrasound probe is inserted into the vagina and the cervix is imaged on a screen.
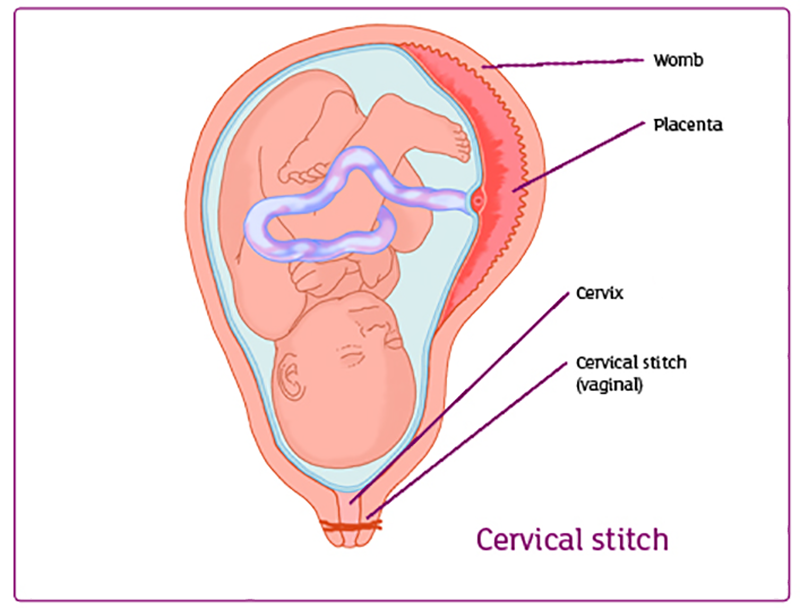
If the cervix shows signs of opening up, the care provider may recommend the person to have a cerclage at that point.
-
Cervical Insufficiency
This is an uncommon condition, sometimes known as cervical incompetence, where the cervix opens (dilates) without the patient having contractions. Cervical insufficiency can be a cause of miscarriage in the second trimester. If someone has miscarried in the second trimester in the past with out having painful contractions, the care provider may recommend her have a cerclage in this pregnancy. A cerclage is a stitch that is placed around the cervix to keep it tightly closed, rather like a drawstring around the neck of a balloon. An alternative to a cerclage, in some cases, is to be monitored with a transvaginal ultrasound weekly or every other.
Sometimes changes in the cervix are noted during a routine, second-trimester ultrasound. In this case, if the person has not had a miscarriage before, it is controversial whether placing a cerclage is helpful. The care provider will review the risks and benefits with this or refer the person to a specialist for consultation